Chapter VIII
BLUEPRINT FOR A REVOLUTION
We have no doubt about the contribution of medical research to better quality of life and longevity. Nevertheless, in this book we illustrate how the existing ‘drivers’ for research – commercial and academic – have not done enough to identify patients’ priorities. Healthcare will always be full of uncertainties, of greater or lesser importance, and where better to address them than the NHS, in which all of us have a stake. So how do we bring about a revolution in which uncertainties in everyday healthcare are not dodged, but taken up as challenges; in which research to test treatments becomes a vital part of good healthcare?
Before outlining our blueprint for this revolution, let us give you a feeling for what we hope might happen in the routine setting of a general practice in future.
OUR BLUEPRINT
Taken individually, none of the suggestions that follows is revolutionary, or even novel. Taken together and promoted jointly by patients and clinicians, our seven action points constitute a blueprint for a revolution in the use and testing of treatments.
1. Encourage honesty when there are uncertainties about the effects of treatments.
Admitting uncertainty is often hard for health professionals, and it is sometimes not welcomed by patients. As a result, people are sometimes being given a false sense of security. If clinicians and patients are to work together successfully for more efficient assessment of treatment effects, both must be more ready to acknowledge that inadequately evaluated treatments can do substantial harm; they must become more familiar with the methods needed to obtain reliable evidence. We need to find out the best ways of making this happen.
2. Confront double standards on consent to treatment offered within and outside clinical trials.
Clinicians who are prepared to admit uncertainties about the effects of treatments and address them in formal treatment comparisons are subject to more stringent rules for interacting with patients than are their colleagues. When there are uncertainties about treatment effects, participation in controlled trials or other methods of unbiased evaluation should be the norm. We should ensure that participation in research on treatment effects is not presented as a risky endeavour, implying that ‘standard’ practice is always effective and safe.
3. Increase knowledge about how to judge whether claims about treatment effects are trustworthy.
A condition for change is greater public engagement with the ways in which bias and the play of chance can seriously distort evidence about the effects of treatments. One of the most important features of scientific investigation – recognising and minimising bias – can hardly be regarded as ‘general knowledge’. We need more determined efforts to reduce these important gaps in understanding, and to make these concepts a routine part of education, from school age onwards.
4. Increase the capacity for preparing, maintaining, and disseminating systematic reviews of research evidence about the effects of treatments.
Many of the answers to pressing questions about the effects of treatments can be readily addressed by systematically reviewing evidence that already exists, by keeping such reviews up to date, and by disseminating the results efficiently to professionals and patients. There is a long way to go before the messages from existing evidence are readily available in systematic reviews. We should urge the NHS to make this one of its prime goals, so that reliable information about the effects of treatments is synthesised and made readily accessible throughout the health service.
5. Tackle scientific misconduct and conflicts of interest within the clinical research community.
Many people are astonished to find that researchers are not required to assess systematically what is known already when they seek funding and ethical approval for new research. The consequence is inevitable – poorly designed and frankly unnecessary research continues on a scale that is unacceptable on ethical as well as scientific grounds. We should press research funders and research ethics committees to ensure that researchers do not embark on new research of any kind without referring to systematic reviews of other relevant evidence. Furthermore, biased under-reporting of research is unethical. Researchers should be required to publish the results of all research to which patients have contributed, and to make clear what contribution the new evidence has made to the totality of relevant evidence.
6. Require industry to provide better, more complete, and more relevant evidence about the effects of treatment.
In 2005, the House of Commons Health Committee published a hardhitting report on the influence of the pharmaceutical industry.139 Whenever the power and influence of the drug industry has been challenged in the past, the pharmaceutical giants have responded with near threats to withdraw their research and development activities from the UK and have issued dire warnings about the consequences for the UK economy. Successive governments have listened, capitulated, and done nothing to curb the industry’s excesses. The Committee’s recommendations should not be allowed to fall by the wayside. In particular, we should demand that all clinical trials are registered publicly at the outset, and that all the results are published in full on completion.
7. Identify and prioritise research addressing questions about the effects of treatments which are deemed important by patients and clinicians.
The portfolios of research funders and academic institutions are dominated by basic research that is unlikely to benefit patients in the foreseeable future, and by research directed at maximising profits for industry. Applied research into questions that offer no potential to make money, yet matter to patients, has to fight for a toe-hold, even when it is publicly supported. We should see to it that the NHS does more to identify what questions patients and clinicians are asking about the effects of treatments, and that research funders take account of them in prioritising research to reduce these uncertainties.
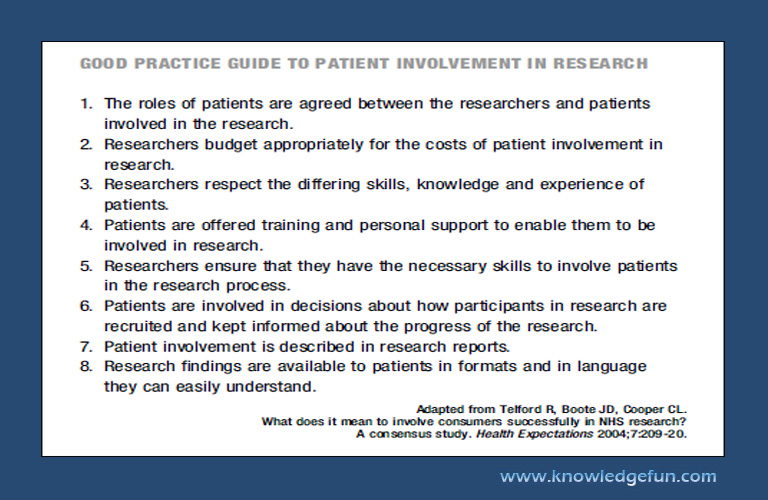
GOOD PRACTICE GUIDE TO PATIENT INVOLVEMENT IN RESEARCH
1. The roles of patients are agreed between the researchers and patients involved in the research.
2. Researchers budget appropriately for the costs of patient involvement in research.
3. Researchers respect the differing skills, knowledge and experience of patients.
4. Patients are offered training and personal support to enable them to be involved in research.
5. Researchers ensure that they have the necessary skills to involve patients in the research process.
6. Patients are involved in decisions about how participants in research are recruited and kept informed about the progress of the research.
7. Patient involvement is described in research reports.
8. Research findings are available to patients in formats and in language they can easily understand.
Adapted from Telford R, Boote JD, Cooper CL.
What does it mean to involve consumers successfully in NHS research?
A consensus study. Health Expectations 2004;7:209-20.
IN CONCLUSION
A revolution in testing treatments is long overdue. If professionals and patients act together, the steps that we advocate are eminently practicable. You the readers should clamour for change – now.