Chapter VI
LESS RESEARCH, BETTER RESEARCH,
AND RESEARCH FOR THE RIGHT REASONS
An editorial in the British Medical Journal some years ago carried an arresting title: ‘The scandal of poor medical research’. The author called for less research, better research, and research done for the right reasons. In earlier chapters we have shown the kind of things that were bothering him.
LESS RESEARCH
For most of the organisations supporting biomedical research and most of the researchers doing it, their stated aim is straightforward: to contribute information to improve people’s health. But how many of the millions of biomedical research reports published every year really do make a useful contribution to this worthy cause?
Researchers in Bristol decided to pose a fundamental question: ‘To what extent are questions of importance to patients with osteoarthritis of the knee and the clinicians looking after them reflected in the research on this condition?’ They began by convening four focus groups – of patients, rheumatologists, physiotherapists, and general practitioners, respectively. These groups were unanimous in making clear that they did not want any more trials sponsored by pharmaceutical companies comparing yet another non-steroidal anti-inflammatory drug (the group of drugs that includes, for example, ibuprofen) against a placebo (dummy drug). Instead of drug trials, participants in the focus groups wanted rigorous evaluation of physiotherapy and surgery, and assessment of the educational and coping strategies that might help patients to manage this chronic, disabling, and often painful condition more successfully. Of course, these forms of treatment and management offer much less scope than drugs for commercial exploitation so are too often ignored.
How many other fields of therapeutic research would, if evaluated in this way, reveal similar mismatches between the questions about treatment effects that matter to patients and clinicians, and those that researchers are addressing? Other examples (85, 86, 87) lead us to suspect that mismatch is the rule rather than the exception. Minor changes in drug formulation rarely lead to the drugs having substantially new, more useful effects, yet these types of studies dominate research into treatments for arthritis and for other disorders. What a waste of resources!
Clearly this situation is unsatisfactory, so how has it come about? One reason is that what gets studied by researchers is distorted by external factors. The pharmaceutical industry, for example, does research for its primary need – to fulfil its overriding responsibility to shareholders, not to patients and clinicians. Businesses are driven by large markets – such as women wondering whether to use hormone replacement therapy, or people who are depressed, anxious, unhappy, or in pain. Yet only rarely in recent decades has this commercially targeted approach led to important new treatments, even for ‘mass market’ disorders. Rather, within groups of drugs, industry has produced many very similar compounds – so-called ‘me-too’ drugs. This is reminiscent of the days when the only bread available in supermarkets was endless variations on the white sliced loaf. Hardly surprising, then, that the pharmaceutical industry spends more on marketing than on research.
But how does industry persuade prescribers to use these new products rather than existing, less expensive alternatives? A common strategy is to commission numerous small research projects showing that the new drugs are better than giving nothing at all, while not doing any research to find out whether the new drugs are better than the existing ones. Regrettably, industry has little difficulty in finding doctors who are willing to enrol their patients in this fruitless enterprise. And the same doctors often end up promoting the products studied in this way. Drug licensing authorities often make the problem worse by insisting that new drugs should be compared with placebos, rather than with existing effective treatments.
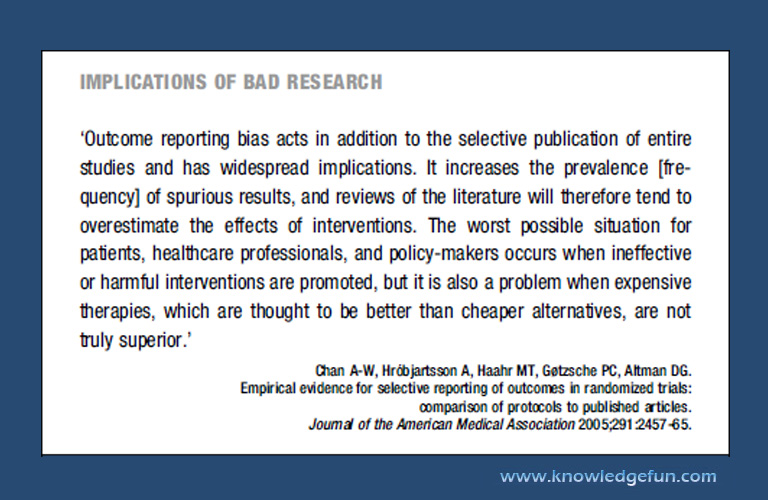
IMPLICATIONS OF BAD RESEARCH
‘Outcome reporting bias acts in addition to the selective publication of entire studies and has widespread implications. It increases the prevalence [frequency] of spurious results, and reviews of the literature will therefore tend to overestimate the effects of interventions. The worst possible situation for patients, healthcare professionals, and policy-makers occurs when ineffective or harmful interventions are promoted, but it is also a problem when expensive therapies, which are thought to be better than cheaper alternatives, are not truly superior.’
Chan A-W, Hro´bjartsson A, Haahr MT, Gøtzsche PC, Altman DG.
Empirical evidence for selective reporting of outcomes in randomized trials:
comparison of protocols to published articles.
Journal of the American Medical Association 2005;291:2457-65.
Commentaries in prestigious medical journals such as The Lancet have drawn attention to the perverse incentives now driving some of those involved in clinical research, and the increasingly dubious relationships between universities and industry. One editorialist in the New England Journal of Medicine asked bluntly ‘Is academic medicine for sale?’
However, commercial priorities are not the only perverse influences on patterns of biomedical research that disregard the interests of patients. Many people within universities and research funding organisations believe that improvements in health are most likely to stem from attempts to unravel basic mechanisms of disease. So, they do research in laboratories and with animals. Although such basic research is unquestionably needed, there is precious little evidence to support this bias towards it. Yet the consequence has been a massive outpouring of laboratory research that has not been properly evaluated to see how relevant it is to patients.